Release date: 2016-09-29
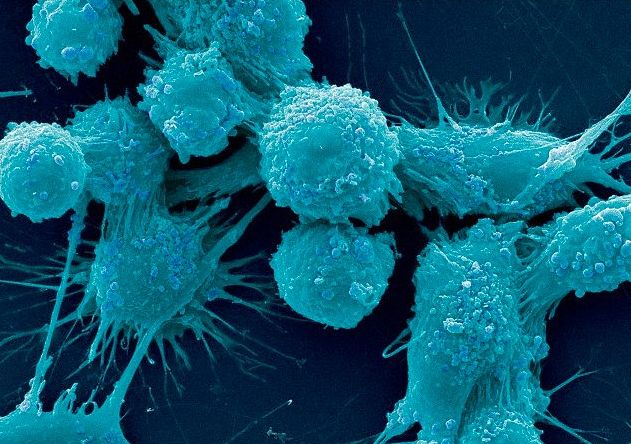
Metabolic changes are one of the important characteristics of tumor cells, which are causally related to the occurrence and development of tumors. German scientist Warburg found that tumor cells preferentially carry out glycolysis even in the presence of adequate oxygen, which provides the corresponding energy for tumor cells and also provides for the synthesis of biomacromolecules. The desired precursor, this is the famous Waberg effect.
In metastatic tumors, scientists also found that glucose metabolism is different, fatty acid over-accumulation and other metabolic reactions are different from normal cells. Of course, studies have also confirmed that targeting tumor cell metabolism is a positive and effective direction for anti- tumor metastasis, and some results Has been applied to clinical treatment.
In this article, Xiaobian compiled the research progress related to tumor metabolism in recent years , and studied with you.
[1] PNAS: Discover new tumor metabolic mechanisms
Doi: 10.1073/pnas.120324410
Recently, James M. Phang, a researcher from the Frederick National Cancer Institute in the United States, found that the oncogenic transcription factor c-MYC can alter the metabolic process between proline and glutamine and promote the regulation of c-MYC. Cell proliferation and metabolic response. Relevant research results were published on May 21st in the Proceedings of the National Academy of Sciences (PNAS).
The study found that in addition to glycolysis, the oncogenic transcription factor c-MYC also stimulates the metabolism of glutamine. By up-regulating glutaminase (GLS), energy production is promoted, and as a result, proliferation of cancer cells is promoted.
It is well known that glutamine can be converted to glutamic acid by GLS and becomes an important energy source after entering the tricarboxylic acid cycle. However, it is rarely known that glutamate can be converted to proline by 5-carboxylic acid Δ1-pyrroline (P5C). This study found that some of the intracellular effects induced by MYC are due to the regulation of proline metabolism by MYC.
Proline oxidase, also commonly known as proline dehydrogenase (POX/PRODH), is the first enzyme in the proline catabolism pathway and a mitochondrial tumor suppressor that inhibits cells. Proliferation and induce apoptosis.
[2] Nature: Metabolic reprogramming can cause specific cancers to subside
Doi:10.1038/nature13910
Recently, researchers from the MD Anderson Cancer Research Center in Texas, USA, found that a family member of the tumor suppressor gene p53 or a tumor that promotes p53 deficiency is rapidly declining. The related research was published in the internationally renowned journal Nature.
Studies have shown that diabetes drugs that affect the same gene-protein pathway may be effective in treating cancer; researcher Elsa R. Flores said that in vivo studies have shown that p63 and p73 can be controlled to up-regulate or increase human amylin (IAPP) Level, Iapp is a key protein in the body that metabolizes glucose, which is currently used in some drugs for the treatment of diabetes.
P53 is altered in most human cancers, and reactivation of p53 in mice inhibits tumor development, but the use of it is now very difficult to treat, the researchers said, by changing the p53 family members p63 and p73 Perhaps the goal of treating cancer can be achieved. In this study, the researchers described two versions of p63 and p73. The first version is the transactivation domain, which is structurally and functionally similar to p53, which can effectively inhibit cancer; another version is the deletion activation region. Inhibition of p53 blocks tumor growth, and the activation region is a region containing a specific protein, such as a transcription factor that can downregulate cellular effects in the future.
[3] Cell Cell Metab. Targeting tumor energy metabolism therapy "has a long way to go"
Doi:10.1016/j.cell.2015.12.034
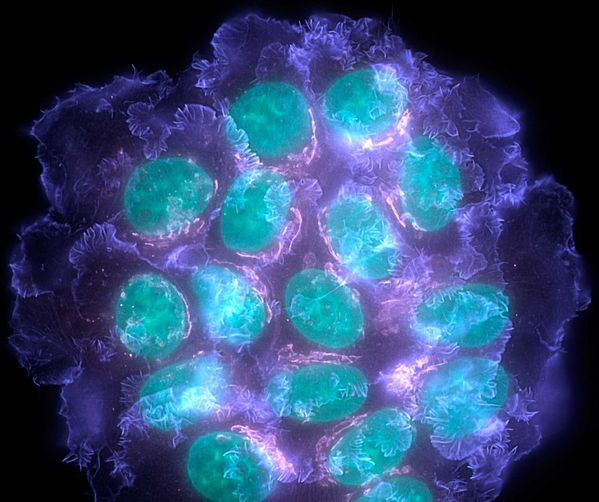
The energy metabolism of tumor cells changes. Compared with the oxidative phosphorylation (OXPHOS) of normal tissue cells, cancer cells choose to activate another energy metabolism method in order to maintain survival and meet the needs of biological macromolecules: aerobic sugar Aerobic Glycolysis.
At present, the research on the energy metabolism of tumor cells is very hot. Scientists hope to systematically use the characteristics of their metabolism to find potential drug targets in the tumor energy metabolism pathway, so as to achieve the purpose of controlling cancer.
But so far, there are still many limitations to this strategy, such as metabolic heterogeneity in tumors, and other metabolic compensation pathways; these strategies still have unpredictable side effects and require strict classification of cancer patients in different situations. Standards and so on.
In two recent articles published in Cell and Cell Metabolism, researchers have proposed two other major obstacles in the use of targeted tumor energy metabolism for clinical treatment. The first is the metastatic heterogeneity of cancer cells in tumors. Second, our current research on tumor metabolism can not simulate the energy metabolism of the real environment of tumors in vivo, so the data obtained is different from the real situation and is not credible.
[4] Cancer Res: New metabolic model drives brain tumors
Doi:10.1158/0008-5472.CAN-12-1572-T
Recently, researchers at Moffett Cancer Center have discovered a new metabolic model of glioma, which is helpful for personalized treatment of tumors.
Related research papers were published in the October issue of Cancer Research, the American Association for Cancer Research. According to the researchers, changes in basic metabolism may drive the growth of the most aggressive tumor type glioblastoma in gliomas.
This study is the first to describe all metabolomics information for glioblastoma. The use of metabolomics to quantitatively evaluate metabolites in a biological system allows researchers to identify key metabolic pathways that drive these tumors to grow. The results of the study led us to further understand the underlying biology of glioblastoma, which seems to be of interest in improving the prognosis of glioma.
[4] Nature: Major discovery! Discover new metabolic switches that promote cancer survival
Doi:10.1038/nature17393
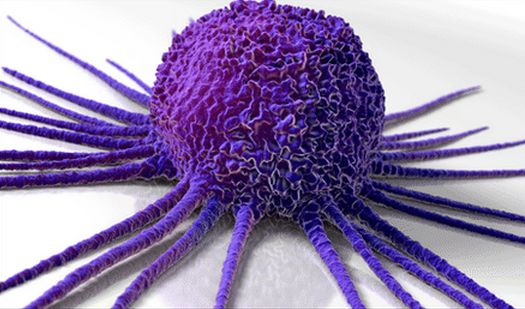
In a new study, researchers from the Children's Medical Center Research Center (CRI) at the University of Texas Southwestern Medical Center identified a new metabolic pathway that aids cancer in conditions that are fatal to normal cells. The cells grow and multiply. The relevant research results were published online in the Nature Journal on April 6, 2016, and the title of the paper is "Reductive carboxylation supports redox homeostasis during anchorage-independent growth".
Dr. Ralph DeBerardinis, author of the paper and director of the Department of Pediatric Genetics and Metabolism at the Southwestern Medical Center of the University of Texas, said: "People have long believed that if we can target tumor-specific metabolic pathways, then it is possible to develop an effective treatment for cancer. Methodology. This study found that two very different metabolic processes are associated with a particular need for cell adaptation and stress associated with cancer progression."
[5] Cell Reports: Metabolic Mechanism of Mitochondrial Defective Tumor Cells
Doi:10.1016/j.celrep.2014.04.037
Recently, the University of Texas Southwestern Medical Center Children's Medical Center Institute has obtained a groundbreaking research discovery. A research team led by Dr. Ralph DeBerardinis reveals the "password" of atypical metabolic pathways that make certain cancerous tumors grow and develop. "Provides a possible "road map" for combating this cancer."
Related research results were published in the journal Cell Reports, and Dr. DeBerardinis et al. described the key role of the trigger mechanism that led to the reverse operation of a series of energy-generating chemical reactions known as the Krebs cycle.
With this discovery, the researchers learned that there are specific enzymes that work together to reverse the energy-generating chemical reaction, Dr. DeBerardinis said: The identification of this mechanism can provide a drug target that will rely on a reverse reversal energy generation pathway to support growth. The tumor. This type of tumor is often found in the brain, lungs, and kidneys and is often difficult to treat because cancer cells use atypical pathways that appear to be resistant to existing treatments such as chemotherapy.

[6] Cancer cell: myc dysregulation promotes metabolic reprogramming and tumorigenesis requires a factor
Doi:10.1016/j.ccell.2014.11.024
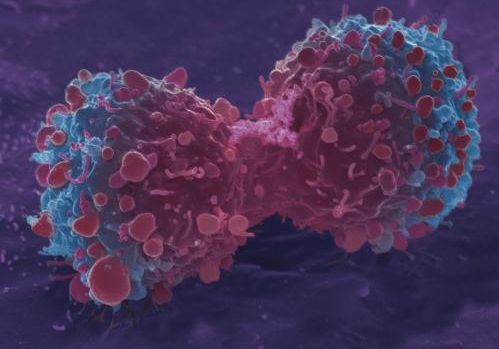
Recently, the famous international biology journal cancer cell published a new research result of American scientists. They found that the reprogramming of oncogene myc to tumor metabolism requires the joint action of myc superfamily member mondoA. This study provides a new strategy for suppressing tumorigenesis.
The researchers point out that when Myc is dysfunctional, it can reprogram cell metabolism at the transcriptional level and promote tumor formation. Patrick A. Carroll et al. found that the oncogene myc also needs members of the myc superfamily, and the role of the nutrient-sensitive transcription factor mondoA promotes tumorigenesis. By knocking down mondoA or a mixture that dimerizes with it, it is possible to block the reprogramming of multiple metabolic pathways induced by myc, leading to apoptosis. The genes co-regulated by myc and mondoA were identified and knocked down. The researchers found that lipid synthesis plays a very important role in maintaining myc-driven tumor survival. Further studies on clinical tumor patients have found that overexpression of myc and mondoA co-regulatory genes is associated with adverse conditions in many cancer patients.
[7] PNAS: an protein that causes aerobic glycolysis in tumor cells
Doi: 10.1073/pnas.1014769108
Researchers from the Peking Union Medical College/Institute of Basic Medical Sciences of the Chinese Academy of Medical Sciences, Xiamen University of Science and Technology, Harvard Medical School and other places have found that proteins that cause aerobic glycolysis in tumor cells help to unravel abnormal growth and metabolism of tumors. The mystery also provides a new strategy for the treatment of cancer. The research was published in the Proceedings of the National Academy of Sciences (PNAS).
The author of the article is Professor Zhang Hongbing, a doctoral tutor at the Institute of Basic Medical Sciences of the Chinese Academy of Medical Sciences, and Professor You Han from Xiamen University. Professor Zhang Hongbing is currently a Distinguished Professor of Peking Union Medical College, a doctoral tutor, and a visiting professor at the Center for Tissue Engineering Research of the Chinese Academy of Medical Sciences. His research interests include tumor signaling pathways and tumor suppressor genes.
Tumor patients are often accompanied by metabolic disorders such as high energy expenditure and weight loss. In the 1920s, German Nobel laureate Otto Waberg discovered that the metabolism of tumor tissue was significantly enhanced. Tumor cells mainly rely on glycolysis for metabolism, and their sugar consumption rate is much higher than that of normal cells. Whether this metabolic characteristic is the cause of cancer or the result of metabolic changes of cancer cells is a problem that has long plagued the medical community.
[8] My scientist Cell research issued a document: cMyc regulates the new mechanism of tumor cell metabolism
Doi: 10.1038/cr.2015.33
Recently, researchers from the University of Science and Technology of China published their latest research progress in the international academic journal cell research. They found that in the state of nutrient deficiency, cMyc can activate the serine synthesis pathway to maintain cancer cell survival and promote cell proliferation, which indicates that in tumor cells. cMyc plays an important role in the metabolic conversion process.
It is well known that cancer cells undergo metabolic reprogramming processes to maintain their own survival and rapid proliferation, but it is still unclear how oncogenes can undergo metabolic transformation under various stress conditions. The researchers found that cancer cells significantly activated the serine synthesis pathway (SSP) in the absence of two major nutrient sources, glucose or glutamine, with an increase in cMYC expression.
The researchers further confirmed that cMYC can up-regulate the expression of several key enzymes in the serine synthesis pathway at the transcriptional level to activate the serine synthesis pathway. Activation of the SSP pathway promotes glutathione synthesis, cell cycle progression, and nucleic acid synthesis, by which cells maintain cell survival in a nutrient-deficient state and promote cancer cell proliferation.
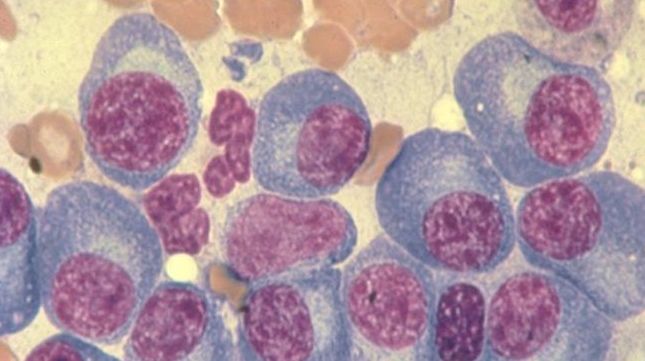
[9] Nature Com: Lymphoma is associated with metabolic damage
Doi:10.1038/ncomms8768
Researchers at the Health Science Center at the University of Texas Medical School in San Antonio found evidence that disruption of metabolism (energy production in cells) is associated with a common, often fatal, type of lymphoma. The discovery was published in the journal Nature Communications.
The topic “There is a link between metabolism and cancer†has been proposed or inferred for a long time, but there is little direct evidence to suggest genetic mutations in metabolic enzymes. Ricardo, MD, said.
"We found that metabolic imbalances can cause cancer," Dr. Aguiar said. The research team consisted of members from the Medical Sciences and Biochemistry Department of the Health Sciences Center. The investigators came from the Southwestern Medical Center of the University of Texas at Dallas and a group of Austrian collaborators who discovered the code D2-hydroxyglutarate dehydrogenase (D2HGDH) The gene is mutated in a cancer called diffuse giant B-cell lymphoma. The mutated lymphoma cells show a lack of a metabolite called alpha ketoglutarate (α-KG), which is necessary for maintaining cell stability and health.
Source: Bio Valley
C200 Trolley Color Doppler Ultrasound System
Feature:
·High definition clear image
·15inch touch Screen LED Screen
·Built-in Battery
·3D/4D imaging(option)
·Support phased array probe(option)
·Abundant functions, Multilingual
·Hardisk, USB storage
·Generous and exquisite appearance
Specifications:
1. Imaging Modes:
lB, B|B, 4B, B|M, M
lColor Doppler (CFM)
lPower Doppler (PDI)
lDirectional Power Doppler (DPDI)
lPulsed Wave Doppler (PWD)
lB+PWD (Duplex)
lB+CFM/PDI/DPDI+PWD (Triplex)
lHigh Pulse Repetition Frequency (HPRF)
lTissue Harmonic Imaging (THI)
SS-100 Touch Screen Trolley Ultrasound Diagnosis B Scanner
Feature:
-Full digital imaging technology
-Crystal-clear Image
-Computer platforms, Abundant functions
-Powerful image and report management
-3D Image Function(optional)
-DICOM display and transfer
-250G large Storage volume
-Broadband Multi-frequency probes
-Compatible with USB laser/inkjet printers
-Pretty and new appearance
-15 inch touch screen color LCD monitor
-Silica gel backlight waterproof keyboard
-8 segment TGC, 16 step zoom
-Complete application software packages
-Can work with external battery(option)
-2 probe connector
-Can be fold, the transportation is convenient and lower freight
-Multiple language: English, French, German, Spanish, Russian, Italian, Portuguese, etc.
Specification:
-D-Maximum Scanning Depth: max.250mm
-Multi-frequency: 5 segment frequencies
-Zoom: 10 ratio, 1.5, 2.0, 2.5, 3.0, 3.5, 4.0, 4.5, 5.0, 5.5, 6.0
-Image gray scale: 256 level gray scale
-Cine Loop: max.1024 frames
-Scanning mode: B, 2B, B/M, M, 4B, 9B, ZOOM;
Real-time Zoom on B mode
-Image processing: Pre-processing, after-processing, dynamic range, frame rate, line average, edge;
enhancement, Black/White inversion; Gray scale adjustment, contrast, brightness, γ revision.
-Gain: gain: adjustable between 0-100dB;
Time gain control(TGC): 8 segment adjustment, B, M adjustment separately.
-Monitor: 15 inch touch screen color LCD monitor
-Supported output apparatus: U-Disk, Laser/ink printer, video printer, VGA
-Measurement and calculation(human):
B mode: distance, circumstance, area, volume, angle, ratio, stenosis, profile, histogram;
M mode: heart rate, time, distance, slope and stenosis;
Gynecology measurement: Uterus, cervix, endometrium, L/R ovary;
Obstetric: gestation age, fetal weight, AFI;
Cardiology: LV, LV function, LVPW, RVAWT;
Urology: transition zone volume, bladder volume, RUV, prostate, kidney;
Small parts: optic, thyroid, jaw and face.
-Measurement and calculation(veterinary):
Cattle: BPD, CRL, TD; Horse: GA; Dog: GS; Cat: HD, BD;
Sheep: BPD, CRL, TD
-Image store: by 250G hardisk or USB disk
-Print: by USB laser/inkjet printers
-DICOM3.0, medical digital imaging and communication
-Probe Connector: 2
-Weight: Around 28kg
Trolley Ultrasound Scanner,Trolley Type Ultrasound Machine,Color Doppler Ultrasound Trolly,B-Ultrasound Scanner Trolley
Guangzhou Sonostar Technologies Co., Limited , https://www.sonoeye.com